Integrative group visits emerge as key tool in community healthcare
November 16, 2017
 by John Weeks, Publisher/Editor of The Integrator Blog News and Reports Editor’s note: This analysis article is not edited and the authors are solely responsible for the content. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of Integrative Practitioner. Two recent media releases underscore the emerging importance of integrative group visits in meeting the needs of the underserved in community health. One, from researchers at Boston Medical Center, found positive clinical outcomes from “integrative health group visits.” The other, from a set of community centers in Orange County, boasts that group medical visits provide “more whole person care with less medication for better outcomes.” Integrative health group visits reduce pain for underserved Hispanics The setting was Boston Medical Center’s safety net hospital. The clientele was Spanish-speaking, underserved Latinos with chronic pain. A research group led by Paul Gardiner, MD, MPH chose a novel approach. Why not introduce multiple potentially beneficial therapeutic approaches to the populations via a group, rather than one-on-one. The team adapted an integrative health group visit model for this population that is typically challenged to pay for such services or to regularly maintain a multi-week schedule of a multi-hour class. Their integrative group service found significant changes on pain, fatigue and depression.
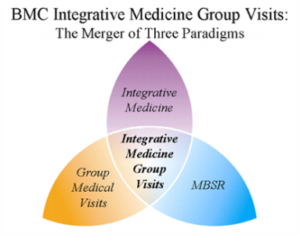
by John Weeks, Publisher/Editor of The Integrator Blog News and Reports Editor’s note: This analysis article is not edited and the authors are solely responsible for the content. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of Integrative Practitioner. Two recent media releases underscore the emerging importance of integrative group visits in meeting the needs of the underserved in community health. One, from researchers at Boston Medical Center, found positive clinical outcomes from “integrative health group visits.” The other, from a set of community centers in Orange County, boasts that group medical visits provide “more whole person care with less medication for better outcomes.” Integrative health group visits reduce pain for underserved Hispanics The setting was Boston Medical Center’s safety net hospital. The clientele was Spanish-speaking, underserved Latinos with chronic pain. A research group led by Paul Gardiner, MD, MPH chose a novel approach. Why not introduce multiple potentially beneficial therapeutic approaches to the populations via a group, rather than one-on-one. The team adapted an integrative health group visit model for this population that is typically challenged to pay for such services or to regularly maintain a multi-week schedule of a multi-hour class. Their integrative group service found significant changes on pain, fatigue and depression.  The model developed by Gardiner’s team focused on teaching self-management techniques and on enhancing patients' social support networks. The course of care combined complementary and integrative medicine, medical group visits, and mindfulness-based stress reduction techniques to address several health issues such as insomnia, stress, and depression. The team recently published their positive results in JACM/The Journal of Alternative and Complementary Medicine as “The Latino Integrative Medical Group Visit as a Model for Pain Reduction in Underserved Spanish Speakers.” Said Gardiner, in a media release accompanying the publication: “In the United States, there is a health disparity in the treatment of chronic pain. Medical group visits provide non-pharmacological strategies and provide more access to care.” (A Health Affairs commentary on integrative health group visits by Gardiner’s colleague Katherine Gergen Barnet, MD is here.) Orange County Clinic Delivers Integrative Model for Group Medical Visits
The model developed by Gardiner’s team focused on teaching self-management techniques and on enhancing patients' social support networks. The course of care combined complementary and integrative medicine, medical group visits, and mindfulness-based stress reduction techniques to address several health issues such as insomnia, stress, and depression. The team recently published their positive results in JACM/The Journal of Alternative and Complementary Medicine as “The Latino Integrative Medical Group Visit as a Model for Pain Reduction in Underserved Spanish Speakers.” Said Gardiner, in a media release accompanying the publication: “In the United States, there is a health disparity in the treatment of chronic pain. Medical group visits provide non-pharmacological strategies and provide more access to care.” (A Health Affairs commentary on integrative health group visits by Gardiner’s colleague Katherine Gergen Barnet, MD is here.) Orange County Clinic Delivers Integrative Model for Group Medical Visits  The October 19, 2018 media release from a multi-community clinic initiative called Live Healthy OC distinguished itself this way for the integrative health community: “While our clinics are not the first to incorporate integrative health modalities into their model of care, we are the first to do so with this magnitude through a network of clinics that have the potential to touch more than 33,000 patients in our community.” The speaker was project manager Rhonda M. Smith. While located in a county south of Los Angeles known for its wealth – the “OC” stands for Orange County – most clients are from underserved and frequently Latino populations. The Live Healthy OC approach includes an expansive form of group medical visits into which integrative concepts and therapies are introduced. Among these are nutritional workshops and “holistic health solutions like yoga, acupuncture, tai chi, and meditation.” A participant patient is quoted in the release speaking of the value he gained in learning from his peers and “the similar struggles we share.” He adds that in the visits he has “learned so much about natural remedies to reduce my sugar levels and have incorporated aloe vera and chia in my diet now.”
The October 19, 2018 media release from a multi-community clinic initiative called Live Healthy OC distinguished itself this way for the integrative health community: “While our clinics are not the first to incorporate integrative health modalities into their model of care, we are the first to do so with this magnitude through a network of clinics that have the potential to touch more than 33,000 patients in our community.” The speaker was project manager Rhonda M. Smith. While located in a county south of Los Angeles known for its wealth – the “OC” stands for Orange County – most clients are from underserved and frequently Latino populations. The Live Healthy OC approach includes an expansive form of group medical visits into which integrative concepts and therapies are introduced. Among these are nutritional workshops and “holistic health solutions like yoga, acupuncture, tai chi, and meditation.” A participant patient is quoted in the release speaking of the value he gained in learning from his peers and “the similar struggles we share.” He adds that in the visits he has “learned so much about natural remedies to reduce my sugar levels and have incorporated aloe vera and chia in my diet now.”  Live Healthy OC also positions itself as providing positive outcomes for its practitioners. One, Marco Angulo, MD, a chief medical officer at one of the facilities, says the visits give him a renewed sense of purpose: “This is why I went to medical school. Instead of jumping from room to room, prescribing medicine, and sending people on their way, the Group Medical Visit model lets me spend more time with my patients, teaching them how to manage their own health needs and giving them the tools to make better choices.” The project is backed through the end of 2018 by a consortium of funders including the Samueli Foundation, the Susan Samueli Center for Integrative Medicine and the UC Irvine School of Family Medicine Residency. While the release references positive outcomes, no quantitative data were provided.
Live Healthy OC also positions itself as providing positive outcomes for its practitioners. One, Marco Angulo, MD, a chief medical officer at one of the facilities, says the visits give him a renewed sense of purpose: “This is why I went to medical school. Instead of jumping from room to room, prescribing medicine, and sending people on their way, the Group Medical Visit model lets me spend more time with my patients, teaching them how to manage their own health needs and giving them the tools to make better choices.” The project is backed through the end of 2018 by a consortium of funders including the Samueli Foundation, the Susan Samueli Center for Integrative Medicine and the UC Irvine School of Family Medicine Residency. While the release references positive outcomes, no quantitative data were provided.  Comment: For those who use the Quadruple Aim as a yardstick - remember when this was a potential direction for the US medical industry? – these programs strike rich chords. First, there are both the patient engagement and experience outcomes boasted by both models and proved in the Gardiner. Second, there are the commonsense cost savings form work on life style change and efficiencies on practitioner costs per patient contact hour of the group delivery model. Finally, and often overlooked despite the problematic levels of stress and burnout that riddle virtually all medical delivery, there is the pleasure in patient contact and re-engagement of purpose noted by Live Healthy OC’s Angulo. The recent National Associations of Attorneys General's petition to insurers to start covering more of these non-pharmacologic, integrative services should be steering insurers toward integrative group programs. For that matter, so should the National Academy of Medicine which has engaged a major initiative related to burnout. The trouble with commonsense, as Voltaire has been credited with saying, is that it’s not so common.
Comment: For those who use the Quadruple Aim as a yardstick - remember when this was a potential direction for the US medical industry? – these programs strike rich chords. First, there are both the patient engagement and experience outcomes boasted by both models and proved in the Gardiner. Second, there are the commonsense cost savings form work on life style change and efficiencies on practitioner costs per patient contact hour of the group delivery model. Finally, and often overlooked despite the problematic levels of stress and burnout that riddle virtually all medical delivery, there is the pleasure in patient contact and re-engagement of purpose noted by Live Healthy OC’s Angulo. The recent National Associations of Attorneys General's petition to insurers to start covering more of these non-pharmacologic, integrative services should be steering insurers toward integrative group programs. For that matter, so should the National Academy of Medicine which has engaged a major initiative related to burnout. The trouble with commonsense, as Voltaire has been credited with saying, is that it’s not so common.



















SHARE