Navigating stress, pain, and addiction with functional medicine
Pain, stress, and addiction cannot be separated from each other, said David Haase, MD, at the 2019 Institute for Functional Medicine Annual International Conference in San Antonio, Texas.
Occurrences of pain, stress, and addiction are on the rise and are linked in both occurrences and causes. On average, 130 Americans die every day from an opioid overdose; the World Health Organization dubbed stress the health epidemic of the 21st century; roughly 20-40 percent of Americans suffer with chronic pain; and the prevalence of addictive substances and behaviors, such as tobacco, gambling, shopping, and eating, has also increased by up to 15 percent, Hasse said.
But how did we get here? Hasse looked at the opioid crisis as an example—there was a common misconception in the medical community that chronic pain patients were unlikely to become addicted to opioid medications. Therefore, opioids were used for any pain condition, not strictly acute or terminal pain, he said.
The current “gold standard” for treatment of opiate addiction, Hasse said, is “medication-assisted treatment combined with psychosocial therapies and community-based recovery supports.” The functional medicine approach to the triple epidemics of pain, stress, and addiction focuses on the intersection of these diseases and understands that they are linked in not only occurrences and causes, but in solutions.
To the extent that we make something a disease, that is the extent to which we may apply treatment in the world of medicine, Hasse said. To the extent we neglect to focus on function, we are trapped in a linear world of diagnose and treat, of disease and medication, of hallucinated simplicity of cause and effect, he said.
From a functional medicine perspective, pain, stress, and addiction come from a combination of genetics, environment (toxins, diet, poverty, relationships, etc.), and phenotype (outcome of prior gene-environment interactions). Functional medicine asks how and why illness occurs and restores health by addressing the root causes of disease for the individual. The functional medicine model is an individualized, patient-centered, science-based approach that empowers patients and practitioners to work together to address the underlying causes of disease and promote optimal wellness.
There is multi-factorial causation of pain, stress, and addiction, Hasse said. “It takes bravery to ask about the why behind the why behind the why,” he said.
Naming a disease does not equal understanding the system, he said. Though we’ve come to understand pain, stress, and addiction as diseases, practitioners need to address the whole person, following the functional medicine matrix. The matrix organizes a patient’s clinical imbalances, looking at emotional, mental, and spiritual health at the center, while also considering assimilation, structural integrity, communication, transport, biotransformation and elimination, energy, and defense and repair. The functional medicine matrix also aims to retell the patient’s story, understanding antecedents, triggering events, and mediators or perpetuators. In addition, the matrix includes modifiable personal lifestyle factors:
- Sleep and relaxation
- Exercise and movement
- Nutrition
- Stress
- Relationships
Treated disease does not equal well-function, Hasse said. Practitioners need to focus on helping patients achieve well-function—purpose, comfort, focus, joy, energy, contribution, peace, resiliency, and, above all, connectedness. Hasse offers a functional systems pain, stress, and addiction treatment plan:
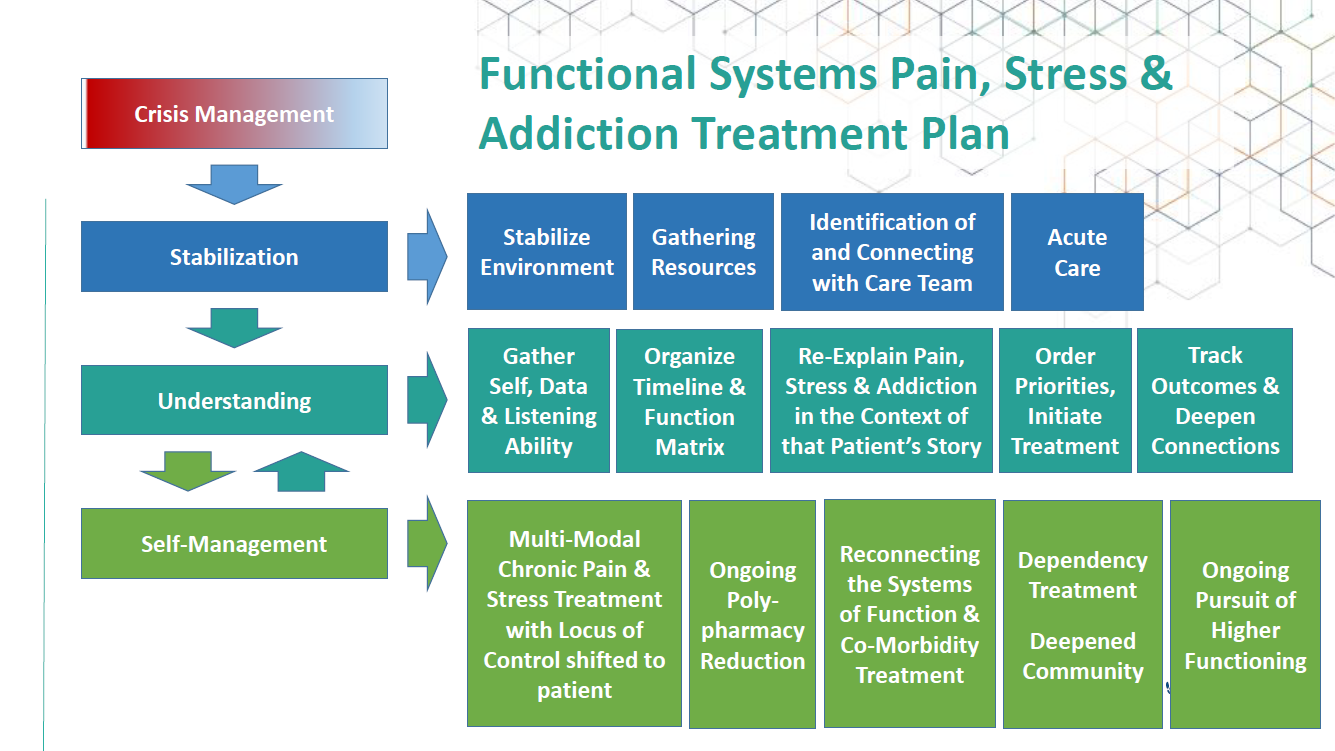
Photo courtesy of the Institute for Functional Medicine.
“We have to be thinking about the whole [person],” said Hasse. "The solutions we are after are connection. We have the opportunity to think about how it is all connected."
Editor’s note: This article is part of Integrative Practitioner’s live coverage of the 2019 Institute for Functional Medicine Annual International Conference. For a full list of coverage, click here.




















SHARE