Primary Cardiovascular Prevention through the lens of integrative medicine
By Regina Druz
Atherosclerotic cardiovascular disease (ASCVD) remains the leading cause of mortality and morbidity in the U.S. and worldwide. Considering that lifestyle efforts may prevent over 80 percent of cardiovascular disease, it is imperative that integrative practitioners are aware of the recently released American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines on Primary Cardiovascular Prevention.
First, definitions of prevention. Primordial prevention refers to prevention of development of the risk factors-, such as hypertension, dyslipidemia, and diabetes, traditionally associated with development of the cardiovascular disease. Primary prevention refers to prevention of the first cardiovascular event in individuals with one or more cardiovascular risk factors. Secondary prevention refers to prevention of a subsequent event in individuals who survived their first cardiovascular event.
In the guidelines, the American Heart Association (AHA) defines ideal cardiovascular health that uses seven metrics collectively called “Life’s Simple 7″. In addition to the seven metrics, guidelines provide suggestions on the use of aspirin. The Simple 7 include:
- Not smoking
- Healthy weight
- Adequate physical activity
- Balanced healthy diet
- Achieving target values for cholesterol, blood pressure, and blood glucose
The guidelines also provide a simple, structured “ABCDE” checklist (Figure 1):

Image by the American Heart Association
Assess Risk and Aspirin Use
Guidelines emphasize that the best risk-reducing strategy for asymptomatic patients starts with assessment of their ASCVD risk. However, risk assessments are based on population cohort estimates and are limited by age range, which is 40 to 75 years old, and that they are a statistical estimation of short-term 10-year ASCVD risk using the race- and sex- specific pooled cohort equations (PCE) and lifetime risk with no time points in between.
Given the limitations of population-based risk estimates, estimated ASCVD risk should be interpreted within the context of the patient’s individual circumstances. The PCE either significantly overestimates or underestimates ASCVD in about half of individuals in the 5-20 percent 10-year ASCVD risk range.
The PCE are based on traditional risk factors and do not allow for any additional or novel risk modifiers, such as the impact of microbiome, inflammation, and immune activation, as well as the role of stress perception. All of these have been the focus of research in both the traditional cardiology community and the integrative medicine realm. Testing for subclinical coronary disease may be useful for further risk personalization, as was referred to in my previous article. Use of nattokinase may potentially be of value although not proven by studies.
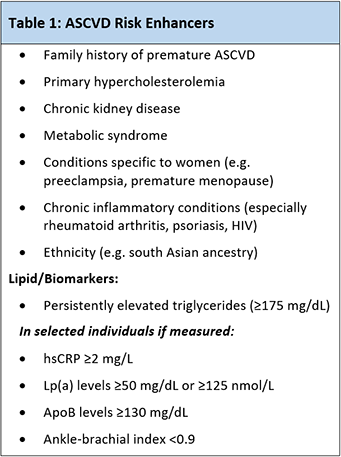
Image by the American Heart Association
While aspirin was previously used routinely for primary ASCVD prevention, it is no longer recommended unless there are additional risk enhancers and the risk of bleeding is low.
Notice that in integrative and functional medicine practice a variety of approaches allow to modify several of the important risk enhancers. Specifically, all nearly all of the lipid/biomarker categories (Lp(a) may be the least modifiable) as well as metabolic syndrome, primary hypercholesterolemia, chronic inflammatory conditions, and vascular reactivity due to underlying root causes in women and those with family history of premature ASCVD are modifiable.
Blood Pressure
The emphasis in blood pressure recommendation is based on 2017 guidelines and emphasizes the importance of lifestyle modifications as the starting intervention for those with elevated blood pressure and a necessary adjunct to pharmacologic therapy when it is indicated. Non-pharmacological therapy in the form of weight loss, a heart-healthy dietary pattern, sodium reduction, dietary potassium supplementation, and increased physical activity with a structured exercise program and limited alcohol is recommended for all adults with elevated blood pressure or hypertension.
Seeing blood pressure as a marker of underlying abnormalities related to metabolic, inflammatory, immune and toxic exposures, such as heavy metals as well as hormonal imbalance issues allows to provide a personalized lifestyle intervention. Assessing for endothelial dysfunction through nitric oxide strip testing and/or brachial reactivity testing (EndoPAT) is helpful serially.
Cholesterol and Cigarettes
The recommendations for cholesterol defer to 2018 AHA/ACC Multi-society guidelines on the management of blood cholesterol. In most adults between age 40 and 70 years, estimating 10-year ASCVD risk using PCE is the initial step to guide the clinician-patient discussion regarding statin therapy. The exceptions are in adults with diabetes or low-density lipoprotein cholesterol (LDL-C) ≥190 mg/dL.
This second group-those with elevated LDL-C- are a group of patients presumed to be individuals with heterozygous familial hypercholesterolemia. The guidelines do not include recent research that shows the profound impact of lifestyle modifications on such individuals if their polygenic risk scores identify them in the highest risk strata. Individualized lifestyle modification strategies will go a long way.
Behavioral modification is laid out as a cornerstone of the smoking cessation.
Diabetes
Type 2 diabetes mellitus (T2DM) is a prevalent disease and a major ASCVD risk factor. All adults with type 2 diabetes are recommended to follow a tailored heart- healthy nutritional plan to improve glycemic control and weight loss. Guidelines focus on observational data that supports the use of Mediterranean, Dietary Approaches to Stop Hypertension (DASH), and vegetarian or vegan diets to improve weight and glycemic index.
Metformin remains first line therapy for patients with T2DM due to its favorable effect on weight loss, glycemic control, and ASCVD outcomes, as well as its low cost and safety profile. In patients with T2DM and other ASCVD risk factors who require additional glucose lowering, sodium-glucose cotransporter-2 (SGLT-2) inhibitors and glucagon-like peptide (GLP)-1 receptor agonists are now considered reasonable options to reduce cardiovascular disease risk.
Integrative practitioners may try alpha lipoic acid in lieu of metformin and ketogenic diet may potentially provide a benefit similar to SGLT-2 agents although this is based on the biological effects of these agents on cardiac metabolism and not on the research studies.
To address the rising epidemic of overweight and obesity, the guidelines highlight the importance of identifying those at risk and focusing on lifestyle recommendations for weight loss. Calculating the body mass index (BMI) to identify adults with overweight (BMI of 25 to 29.9 kg/m2) or obesity (BMI ≥30 kg/m2) is recommended at least annually.
Measuring waist circumference during office visits is reasonable to identify those with central adiposity and high cardiometabolic risk. For those with overweight and obesity, weight loss is recommended to reduce ASCVD risk and improve other ASCVD risk factors.
Exercise
Exercise and physical activity are important lifestyle factors affecting ASCVD risk. Guidelines emphasize moderate or vigorous intensity exercise and avoidance of sedentary lifestyle.
The guidelines are an important step in bringing lifestyle modifications into realm of medicine. Integrative practitioners are instrumental in personalizing lifestyle modifications to benefit cardiovascular patients.
















